INTRODUCTION
Over the past few decades, laser systems have been found extensive application in various clinical aspects of cosmetic surgery. From use in photocoagulation and vaporization of vascular malformations to removal of epithelial lesions, lasers have become an indispensable tool in surgery.
However, the thermal properties of laser treatment adversely affect the adjacent tissue, thus impacting wound healing and scar formation negatively. This problem has been addressed by the more selective and restrictive destruction of targeted tissue by the more recent laser systems like pulsed and Q-switched lasers matched to the target’s absorption characteristics.
These advances help in expanding the therapeutic spectrum of lasers in the field of cosmetic surgery and improvement in the quality of results achieved.
MODES OF OPERATION OF MEDICAL LASERS
Laser radiation used in dermatology work of the same basic principle but can be varied depending on the system used and the intended application keeping the three core variables in mind:
1. Wavelength
2. Pulse Duration
3. Power
LASER INTERACTION WITH BIOLOGICAL TISSUES
The effects induced by lasers in biological tissues can be categorized as follows:
1. Photothermal effects
2. Photochemical effects
3. Photomechanical
4. Photoablative
TYPES OF LASERS USED IN DERMATOLOGY
GAS LASERS
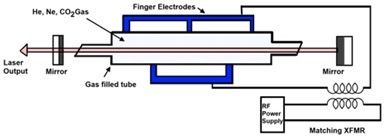
Gas atoms in a glass tube are excited by an electrical charge to produce lasers in this category.
- Carbon dioxide Laser
o The glass tube contains carbon dioxide, helium, and nitrogen (1:8:8)
o This is a continuous wave laser but can be used in pulsed or super-pulsed mode
o It is considered to be the most powerful lasers – reaches a peak power of 80kW- most commonly used between 10-25W in skin surgery.
o The principal chromophore is water for these lasers.
o It can be used in focusing or cutting mode and defocusing or vaporizing mode.
 |
| Carbon dioxide Laser |
- Argon Laser
o Usually used in a continuous wave mode.
o Low efficiency, power: 1-20W therefore the system needs high energy for the pumping system leading to high heat generation.
o Emits light at 6 wavelengths ranging from 442 to 514.5nm
o Light is transmitted along with the fiber by total internal reflection
o Chromophores: Hemoglobin and Melanin
o This leads to selective photo-thermolysis.
o Limitation: Depth of penetration – usually1-2mm of the dermis
- Metal Vapour Laser
o Copper vapor laser: average power: 2-3 W, impulse frequency – 15kHz, and duration 15-20ns. Average energy 0.2nJ/pulse.
o Quasi-continuous beam – due to short pulse length and rapid repetition rate.
o The copper laser emits two harmonic wavelengths: 511nm and 578nm, while gold emits an orange-red beam at 628nm.
DYE LASERS
SOLID STATE LASERS
- Nd: YAG Lasers
o The energy for pumping, in this case, can be optical or low power-output diode laser.
o Nd: YAG can produce tissue reactions almost as deep as 5-7mm of dermis and power is 0.5-95W.
o Due to its scattering effect in tissues, it has applications in coagulation and necrosis.
o For vascular lesions, continuous-wave emission modes are most suitable.
o Recently a Q-switched version using xenon flashlamp known as KTP Laser or Frequency-doubled Q-switched YAG Laser has become available and finds its application in tattoo and pigment removal procedures.
- Ruby Laser
o Active medium Ruby is excited by a flashlamp.
o Short pulses, a red beam
o Used in pigment or tattoo removal – blue and black respond best
 |
| Ruby Laser |
- Alexandrite Laser
o Uses an alexandrite crystal for wavelength propagation
o Wavelength: 755nm, pulse width – 100ns and pulse frequency – 1Hz
o An application being studied: tattoo removal
APPLICATION OF LASERS IN CLINICAL SCENARIOS
VASCULAR-SPECIFIC LASERS
- These lasers target intravascular oxyhemoglobin which has 3 primary absorption peaks 418, 542, and 577 nm.
- Examples: argon (488- 514 nm), KTP (532 nm), copper vapor (578 nm), PDL (585-595 nm), Nd:YAG (532 and 1064 nm), etc
- The argon laser was used for a variety of vascular lesions but has increased the risk of scarring and pigmentation as the exposure interval is longer than the thermal relaxation time leading to nonspecific thermal injury.
- 532-nm KTP avoids purpura and minimizes erythema and has reported good results in the treatment of facial telangiectasias. Disadvantage: decreased tissue penetration.
- More recently, PDLs with longer wavelengths (585, 590, 595, and 600 nm) and extended pulse durations (1.5-40 milliseconds) have been developed.
Fig 1. Port-wine stain in infant – Pre-op (A) and resolution after 8 585-nm pulsed dye laser treatments (B).
Source: Tanzi, Lupton, and AlsterJ Am AcadDermatol July 2003
LASER TREATMENT FOR HYPERTROPHIC SCARS AND KELOIDS
- 585-nm PDL has demonstrated tremendous improvements in scar erythema, pliability, bulk, and dysesthesia.
- Hypertrophic scars show significant clinical improvement after 1 or 2 PDL treatments; however, a greater response may be achieved after multiple treatment sessions using lower energy densities.
- Keloids may require additional laser treatments or the simultaneous use of intralesional corticosteroid or 5-fluorouracil injections.
- Common adverse effects of treatment: cutaneous purpura and transient hyperpigmentation or hypopigmentation. PDL is a first-line treatment for hypertrophic scars and keloids.
PIGMENT-SPECIFIC LASERS
- Pigment Specific Lasers are a common concern of patients presenting to cosmetic clinics.
- Pigments may include melanin-based dermal or epidermal lesions or tattoos.
- High-energy, QS laser systems are melanin-specific which can successfully lighten or eradicate these.
- The continuous and quasi-CW laser systems that have been used for pigment and tattoo destruction include the 488- and 514-nm argon,532-nm KTP,10600nm CO2 lasers, etc.
- CW lasers remove pigment by epidermal denudation and breakdown of the dermo-epidermal junction.
PHOTOEPILATION
- Lasers with wavelengths in the red or near-infrared region are most often used for hair removal.
- Photo epilation lasers target melanin present in the hair shaft, hair follicle epithelium, and heavily pigmented matrix with their deep penetration and selective absorption. The interaction between the laser and follicle is not completely understood yet.
- Active cooling of the skin is used to minimize the adverse effects of heat on the epidermis.
- FDA approved laser systems and IPL sources for photo-epilation include the LP ruby, LP alexandrite, pulsed diode, QS, and LP Nd: YAG lasers and IPL sources.
ABLATIVE LASER SYSTEMS
- Ablative Lasers find application in ablative facial resurfacing, used primarily for rhytides and atrophic facial scars
- Offer the advantage of reduced postoperative morbidity and shorter recovery times.
- Techniques include single-pass CO2 laser ablation and modulated laser systems.
- This treatment method works by ablating the entire epidermis and promotes new collagen formation; leading to the desired effect.
NON-ABLATIVE LASER SYSTEMS
- One of the most recent advances of laser application in the esthetic industry is the development of non-ablative laser systems.
- Non-ablative laser systems employ lasers within the infrared spectrum (1000-1500nm). This wavelength helps in deeper penetration by weak absorption by water.
- Non-ablative lasers do not disrupt the epidermal continuity and create a dermal wound that undergoes collagen remodeling thus inducing resurfacing.
- Although non-ablative lasers have the advantage of no external wound these non-ablative lasers can lead to transient edema, erythema, and hyperpigmentation.
PHOTODYNAMIC THERAPY (PDT)
- Photodynamic therapy PDT uses free radicals formed by light-activated photosensitizers administered exogenously or formed endogenously.
- Photodynamic therapy PDT is finding application in the treatment of skin cancers, solar keratosis, etc.
- The efficacy of this modality is dependent on the nature of photosensitizer, administration modality, light source, and treatment procedure.
- The substrate commonly used for PDT is δ-aminolevulinic acid (ALA).
CONCLUSION
Advances in laser technology have helped in extending their application across various treatment modalities in the cosmetic domain. The superior results and a decrease in post-operative comfort have witnessed an increase in demand by cosmetic surgeons, dermatologists, and improved compliance by patients. Refinements in technology and technique have increased therapeutic choices, improved clinical results, and simplified technical handling. Lasers are slowly replacing conventional scalpel surgery with their multifaceted applications.
REFERENCES
2. Alster TS. Side effects and complications of laser surgery. In: Alster TS. Manual of cutaneous laser techniques. 2nd ed. Philadelphia: Lippincott, Williams & Wilkins; 2000. p. 175-87.

I am really happy to glance at this webpage posts which
ReplyDeleteconsists of lots of useful facts, thanks for providing these kinds of information.
Thank you, always a pleasure to get this great feedback from you!
DeleteThank you, good to know that you liked this article!
ReplyDeleteI am glad to be one of many visitors on this great site (:, thanks for putting up.
ReplyDelete